We recently published an article in Autism Research reporting that autism genes are extremely ancient compared to other genes in the human genome.
Illustration by Alexander Glandien. Courtesy of Spectrum News.
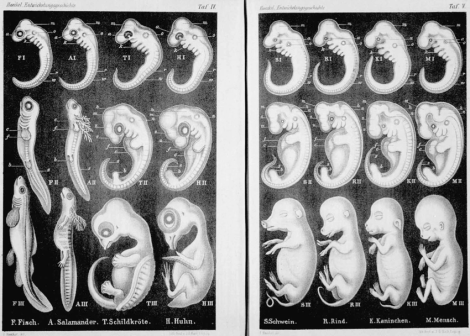
What do I mean by “ancient”? To give a little perspective, the average gene arose during the early chordates, which are organisms that have a notochord. (Chordates also have other defining features but the notochord is most characteristic of this large group.) Chordates include vertebrates such as ourselves, tunicates like sea squirts, and cephalochordates such as the simple fish-like creatures known as lancelets. Chordates first appeared about 530 million years ago. To us as humans who evolved only the last several million years that may seem like a long time ago.
But the average autism gene is even older. Most autism genes evolved during the early bilaterians or even before the development of single-celled fungi like yeast. Bilaterians are animals that have bilaterial symmetry, which is symmetry that occurs along the midline of the body running from head to toe. Bilaterians evolved at least 555 million years ago (mya), if not earlier, and fungi evolved at least 700 mya.
Why is this finding important? Different genes with different functions arose at different periods of evolution. While we don’t currently know the broader evolutionary implication of all of these autism genes, the significant difference in age suggests that they have similar functions and are probably interacting together in an ancient foundational network that’s not just important in brain function but in development of the entire human body. It also suggests that even though the autism spectrum is very genetically and behaviorally heterogeneous, it does have some common roots.
We also found that autism genes are highly conserved (i.e., very sensitive to any kind of mutation), are extremely long, produce very long proteins, these proteins have a larger network of other proteins with which they interact, and the genes contain lots of regulatory elements that help to control gene expression in nuanced ways.
So to recap, this is an ancient group of genes that arose a very long time ago, are conserved across many many organisms suggesting they control very important processes during development, and they’re regulated in many subtler ways, allowing them to function in different cells during different times of development in slightly different ways.
We’re continuing this line of research in the hopes we can better define what these genes are doing as a group in both human development and in many other organisms throughout evolution. In this way, we can better understand what autism is from the biological and evolutionary perspectives. Stay tuned!
(See also Spectrum News for more coverage on our discovery.)

Interesting.
No offense but the more immediately valuable work is being done with the microbiome. Repair the gut and the behavior improves.
“Even 18 weeks after treatment started the children had begun showing reduced symptoms of autism. After two years, only three of them still rated as severe, while eight fell below the diagnostic cut-off point for asd altogether. These eight thus now count as neurotypical.”
economist.com/science-and-technology/2019/05/30/more-evidence-that-autism-is-linked-to-gut-bacteria
Also, one phenotype of autism is certainly immune-system related.
Beyond the brain: A multi-system inflammatory subtype of autism spectrum disorder.
https://www.ncbi.nlm.nih.gov/pubmed/31139876
What is causing such inflammation that damages gut bacteria?
I agree re the microbiome, although I am personally still curious whether it is a cause, symptom, or both, since a process such as inflammation can dramatically alter the gut microbiome. And indeed, when we’re adding certain culturable microbiota back into the diet and improvement is seen, is this because something was truly imbalanced in the gut or because certain microbes are, in effect, anti-inflammatory agents or the like? Many questions need to be addressed still in the science of the microbiome and I suspect we are only at the tip of the iceberg and probably interpreting data too simply. As with all systems, it is probably unappreciably complex.
Re our current work, as I wrote, these genes are not just involved in development of the brain but undoubtedly influence gut development, the immune system, and basically almost every aspect of development in the body. So a mutation in one of these genes can presumably be an important domino in this long line of dominoes that affects autism.
Studying the microbiome I think holds great promise for important subtypes of autism. But biology is rarely that simple. Our genetics work is just looking at another aspect of the larger picture that also includes gut function, inflammation, and the microbiome.
As if every autistic person wants to be cured….
With the microbiome, I’m more interested in general physical well-being for those on the spectrum. Gut problems are definitely prominent, so I’m more interested in improving quality of life for auties. (The science is also intriguing too!)
As a zebra myself, I have major gut issues that are a significant challenge in daily life, trying to endlessly tweak diet, reduce stress, etc. I have more recently added yogurt + culture and have definitely seen an improvement in gut function, so I think it can be a useful additional treatment to add to a long list of approaches of treating GI disorders.
I have gut issues myself, mainly stress related histamin problems.
“I agree re the microbiome, although I am personally still curious whether it is a cause, symptom, or both, since a process such as inflammation can dramatically alter the gut microbiome.”
The mice studies show that it was causal. In a different study they transferred gut bacteria from autistic children into mice and got autistic mice. From the same article above:
“They were looking for the rodent equivalent of asd. And they found it. Most of the young mice harbouring gut bacteria from autistic human donors showed features of autism themselves. These included repetitive behaviours, reduced social and vocal communication with other mice, and restricted movement. In contrast, none of the mice colonised with bacteria from neurotypical people ended up autistic. Dr Mazmanian and his team discovered, moreover, that the intensity of a human donor’s autism was transferred to the recipient mice. If an individual’s symptoms were severe then so, too, were those of mice that hosted his gut bacteria.”
And here is the paper:
Human Gut Microbiota from Autism Spectrum Disorder Promote Behavioral Symptoms in Mice, Cell, May 30, 2019
Click to access S0092-8674(19)30502-1.pdf
This is showing that the triple-hit hypothesis is correct and the double hit hypothesis is (mostly) incorrect. In the triple-hit hypothesis you need:
genetics + environmental trigger + specific brain developmental period.
In the double hit hypothesis, there is no term for the environmental trigger. People who say, “Autism is genetic” as though there is no environmental factor involved should stop saying that. Nor is it some “evolutionary leap” for mankind. For a significant number of people suffering from autism, it is from gut dysbiosis.
I would be cautious in generalizing this to all of autism. Again, the data are intriguing, but blanket theoretical approaches to complex conditions rarely turn out to be useful for all individuals.
With the mouse study, we don’t know if the microbiotia per se are the causative factor in the model or if it’s some other mediating factor. Rodents and primates are closely related in the broader scheme of things, but we are still separated by 70+ million years of evolution, which includes the evolving microbiome. It’s entirely possible that microbiota more prominent in the disturbed gut (e.g., ASD) are not tolerated well by rodents, which leads to an immunological reaction and behavioral disturbances. We already know the immune system is dysregulated in many forms of autism. And I’m sure there’s other possibilities as well.
Don’t get me wrong, the initial study raises fascinating questions and more avenues of study and potential treatment options. But science is cautious for a reason. For instance, is this study replicable across different strains of mouse? There are many studies whose results are entirely dependent on the mouse strain used, which raises questions as to what we’re truly measuring.
I’m not trying to be purposefully argumentative. But as a scientist, my sixth “uh oh” sense starts tingling whenever somebody says to me “This is THE cause of autism” or some other complex condition. At that point, I wanna see data and lots of it. Because it has to outweigh all the other data I’ve seen over my career that may contradict it or, at least, indicate that it’s just not so simple.
That’s fair…though I do think you may be more cautious than is warranted as there are many more studies that support gut bacteria as being causal. I simply picked these two studies because a) they were particularly illustrative and b) this work finally made it to the mainstream news; also, the paragraphs summarizing the studies were accurate and pithy.
My larger point, is that genetics has been fingered as the reason for this tremendous growth in autism cases incorrectly.
My goal is to show that the G term below has been way overblown and the E and GxE terms way underestimated.
G(risk) + E(risk) + GxE(risk) = autism(risk)
Truthfully, I don’t think anyone who studies autism genetics believes that the rise in diagnostic rates has been due to changes in the gene pool itself. There are definitely a subset of cases that have severe mutations (major effect) that are de novo (non-inherited) that seem to be the major risk factor for developing autism (and usually intellectual disability). But these kinds of mutations will always crop up. In fact, serious mutations are extremely common in the larger scheme of things. The majority of embryos are miscarried for these reasons alone. But they are much rarer in the postnatal population.
Some people believe the rise in diagnostic rates is primarily due to changes in diagnostic criteria (which are a big part of it undoubtedly), others suspect it’s that and environmental stressors. I am personally interested in genetics because, as you yourself note, in most cases there should be a genetic vulnerability. Understanding those genes and their larger pathways, as well as the roles they play in development, give us a guide as to what processes are potentially being targeted in more complex forms of autism that may involve environmental exigencies. It also helps give us a better understanding of the underlying biology. Does that make more sense?
It does make sense. The thing is, after $2 billion spent, what do we actually have to show for all this genetic work? From what I can tell, not a single biomarker, not a single treatment.
Has anything come of the genetic angle that I don’t know about?
I personally feel like we’re moving closer to understanding what autism is at the biological level, despite its heterogeneity. Genetics is an important part of the larger puzzle, but I agree it’s not the only part. I have primarily two branches of my research: one is more translatable and involves connective tissue disorders, the immune, nervous, and endocrine systems; and the other branch is genetics. Admittedly, the genetics branch, like the study I reported here, is more basic research. But there’s a lot of basic research that’s very underappreciated because its influences on translational research are more indirect and difficult to measure. But I can promise you that there’s a lot of basic research that has informed my translational research and it’s a vital part of science. We really need both. And even now I’m working with collaborators on a genetics project using the SPARK data in which we’re also going to be looking at complex relationships in phenotype because projects like SPARK nowadays are actually collecting a lot of other information that can give us more insight than just the genetics alone.
Ok, then I haven’t missed anything from a genetic angle (a biomarker or a treatment). I think the people working on the environmental angle have had much more success, such as Dr. Antonucci’s six autism phenotypes:
1. Intoxication: Al, Hg, Pb and other metals cause microglial activation as they travel to and settle in the brain.
2. Bacterial infections: “inflammation of intestinal mucosa, leads to the introduction of bacterial components, including neurotoxins, into the bloodstream, creating oxidative stress as well as microvascularities, especially affecting meningeal vessels, and finally neuronal damage.” — Luc Montagnier, 2008 Nobel Prize Winner for discovering HIV
This is part of all the microbiome work that is getting the recent attention.
3. Viral infections: Injecting live viruses causes some portion to settle in the brain and stomach. They excrete nagalese thereby reducing the child’s native production of GcMAF and inflammation never reduces. According to Dr. Antonucci, about 15% of his autistic patients are chronically infected with the live viruses that were injected into them (primarily MMR).
For both viral and bacterial infections, see:
https://www.mcleanhospital.org/news/mclean-hospital-neuroscientists-find-immune-system-newborns-may-affect-developing-brain
4. Allergic: Al that isn’t being fully excreted causes IL-33 and IgE production; helminth therapy helps with this phenotype.
5. Mitochondrial: This is what got Hannah Poling (mitochondrial damage likely occurred from an earlier shot containing Hg). The mitochondria provide energy to our cells, and are necessary for the Kreb’s cycle, fatty acid oxidation, metabolism of amino acids, and oxidative phosphorylation.
Developmental regression and mitochondrial dysfunction in a child with autism. J Child Neurol, 2006, Poling et al
https://www.ncbi.nlm.nih.gov/pubmed/16566887
6. Autoimmune: One study found that mothers with autoimmune disorders (such as celiac disease, type 1 diabetes, or rheumatoid arthritis) are three times more likely to have autistic kids; other studies uniformly show elevated risk. Vaccinations in the children, which cause an autoimmune response, create the same problem. The likely source of the attack is molecular mimicry of the measles hemagglutinin.
Beyond the brain: A multi-system inflammatory subtype of autism spectrum disorder.
https://www.ncbi.nlm.nih.gov/pubmed/31139876
Anything that attacks/disrupts the brain and causes chronic microglial activation will produce IL-6, which Pineda et al. found was “necessary and sufficient” to cause autism. If the brain also excretes IL-1ß the brain becomes epileptic.
Maternal immune activation promotes hippocampal kindling epileptogenesis in mice.
https://www.ncbi.nlm.nih.gov/pubmed/23907982
Truthfully, I would think most of the immune-related conditions are a single generalizable phenotype and probably has similar underpinnings.
Emily, here is another example of the shift that is underway w/r to autism research.
“Epidemiologic studies have shifted from an exclusive focus on the identification of genetic risk alleles for such disorders to recognizing and understanding the contribution of xenobiotic exposures, infections, and the maternal immune system during the prenatal and early post-natal periods.”
This paper starts from the acceptance that “We now know that even though the BBB isolates the central nervous system (CNS) from factors in the blood, it is a dynamic semipermeable structure. Immune molecules including antibodies can access the CNS during both physiologic and pathologic states.”
Thus, it reviews brain-reactive antibodies that can access the CNS and **maternal** brain-reactive antibodies that can access the CNS.
Maternal Antibody and ASD: Clinical Data and Animal Models, May 28, 2019, Frontiers in Immunology
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6547809/
Yes, the circumventricular organs (CVO) are areas in which the immune system can directly interact with the central nervous system. Certain immunomodulators can also be transported across the BBB via specific channels. Plus, the immune system can indirectly influence the CNS via communication with the PNS. There are many avenues. And there are also many ways that the nervous system can influence activity of the immune system. It’s a complex, elegant crosstalk that is underappreciated in many circles.
Pingback: Love for Science – Made by Stardust·
Pingback: Neurodivergence, Sexuality, Gender, and…the Industrial Age? – Sex Coach Shannon·