Last weekend I attended a Think Tank sponsored by the Autism Research Institute. In attendance were Judy van de Water and Paul Ashwood from the MIND Institute, reporting on some of their latest research efforts. Both of them are probably two of the most renowned immunologists in the field of autism research.

I got a chance to chat with Judy briefly about the state of immune research in autism and to get her take on what percentage of autistic people display evidence of immune dysregulation. (Off-hand, she estimated that maybe up to 60% had features of dysregulation, although that was an informal estimate so don’t quote either of us on that!)
I had been more interested in the immune system in autism years ago but sadly I haven’t kept up with the latest and greatest. So while at the Think Tank, I browsed through some of Judy’s and Paul’s more recent articles. One in particular caught my eye reporting a link between the presence of Metabolic Syndrome in the mothers and immune dysfunction in their autistic children [1]. (The same link was not found in controls.) A subset of the autistic children showed increased markers indicative of inflammation, such as IL-6.
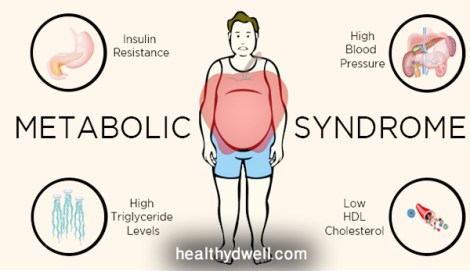
Interestingly, the Metabolic Syndrome is also often associated with fertility issues such as Polycystic Ovarian Syndrome (PCOS), which is believed to result from insulin resistance or type 2 diabetes. And PCOS in the mother has been linked with increased risk for autism in the child [2].
In a new article still currently in press, the MIND Institute team reports that there is a subset of those with autism who have T cell dysregulation, leading to increased activity of the proinflammatory arm of the immune system [3]. What’s more, they found that this subset of children could also be further subdivided: one group showed upregulation of the TH1 proinflammatory arm that targets and protects the body from microbes, meanwhile the second group had upregulated TH2 that’s linked with things like allergies and asthma. Both proinflammatory subgroups showed greater behavioral impairments compared to the autistic subgroup without immune dysfunction, suggesting that the immune system may definitely be playing a key role in the severity of autism symptoms and perhaps their etiologies.
I had often suspected that there may be links between the endocrine and immune systems, especially in relation to the Metabolic Syndrome and autism, but this was the first article I had found shedding direct light on the subject.
The immune system, endocrine disorders and disruption, and brain development… all of these are so interrelated. And immune dysregulation and endocrine disruption are so common in our population that they probably hold considerable explanatory power for a substantial minority/majority of autism risk. Time will tell.

I am interested in immune system irregularities. My wife has immune problems, type 2 diabetes which is under control. Our second daughter was diagnosed with PDD/NOS. She has recovered but was diagnosed with polycystic ovary syndrome. My wife’s sister was diagnosed with gestational diabetes and her son was diagnosed with PDD/NOS and now has a diagnosis of Asperger syndrome.
All of those seem to be very common factors in autism risk. In fact, one of the keynote talks at IMFAR this year was by Irva Hertz-Picciotto who is one of the biggest scientists in autism research who studies environmental factors in autism. She said in her mind, evidence of endocrine/immune disruption in autism and their families is becoming more and more apparent and, at least in her mind, has jumped to the forefront as one of the major common risk factors for autism. Now, that doesn’t mean that it has particularly high penetrance for autism, but it definitely seems to be a common risk background upon which other risk factors act.